If we’re exhausted and wondering why sleep still hasn’t fallen into place after pregnancy and birth, here’s the truth: we’re not doing anything wrong. In 2026, the best sleep solutions for moms and babies are no longer about strict schedules or fixing our babies. They’re about supporting our nervous systems, protecting postpartum recovery, and releasing unrealistic expectations.
This isn’t a guide telling us what we should do. It’s a place to breathe together.
Let’s Start With the Real Problem (The One We Don’t Say Out Loud)
We’re tired.
But not just “need-a-nap” tired.
We’re the kind of tired where:
- Our bodies feel heavy even after resting
- Our minds won’t shut off when the baby finally sleeps
- We lie there listening for breathing
- We quietly wonder, “Is something wrong with me?”
Let’s pause here. Nothing is wrong with us. Postpartum exhaustion isn’t just a lack of sleep; it’s healing + hormones + responsibility + vigilance + love, all happening at once. And most sleep advice skips over us entirely.
Why Sleep Still Feels So Hard Even in 2026
Here’s what we don’t hear enough.
After pregnancy and birth, our nervous systems stay on high alert.
That’s biology, not anxiety.
Our bodies are thinking:
“This tiny human depends on us.”
So even when the baby sleeps, we don’t fully power down.
From both a medical and maternal mental health perspective, this prolonged alert state is closely tied to:
- Postpartum anxiety
- Postpartum depression symptoms
- Difficulty falling or staying asleep
- Racing thoughts at night
That’s why being told to “just sleep” can feel dismissive.
Sleep doesn’t come from trying harder.
It comes from feeling safe enough to rest.
A Small, Real Moment (Because This Is Our Reality)
One mom once shared:
“I wasn’t afraid of being tired. I was afraid of breaking.”
Many of us felt that in our bones.
Because we’re not chasing perfect sleep
We’re trying to survive this season intact.
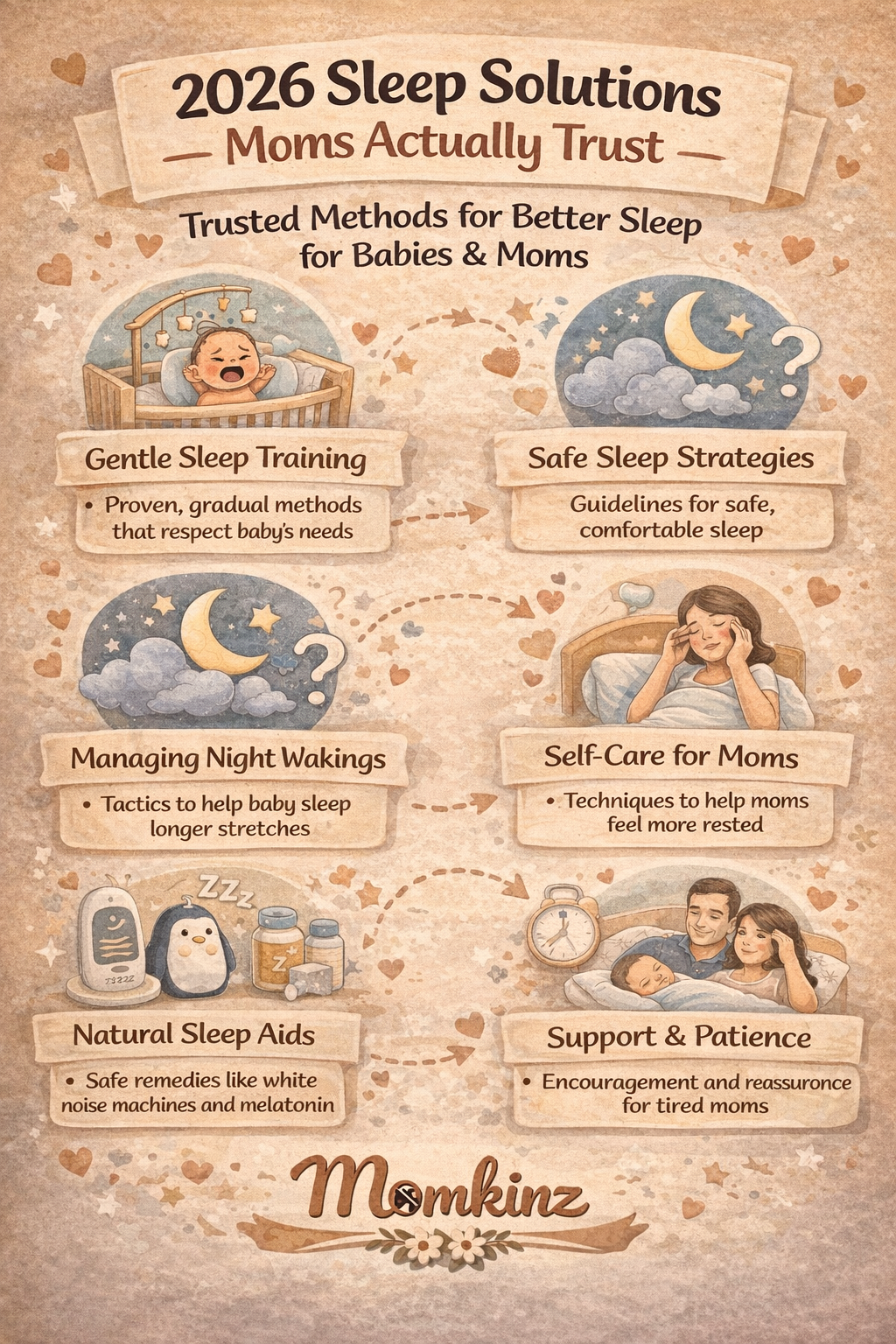
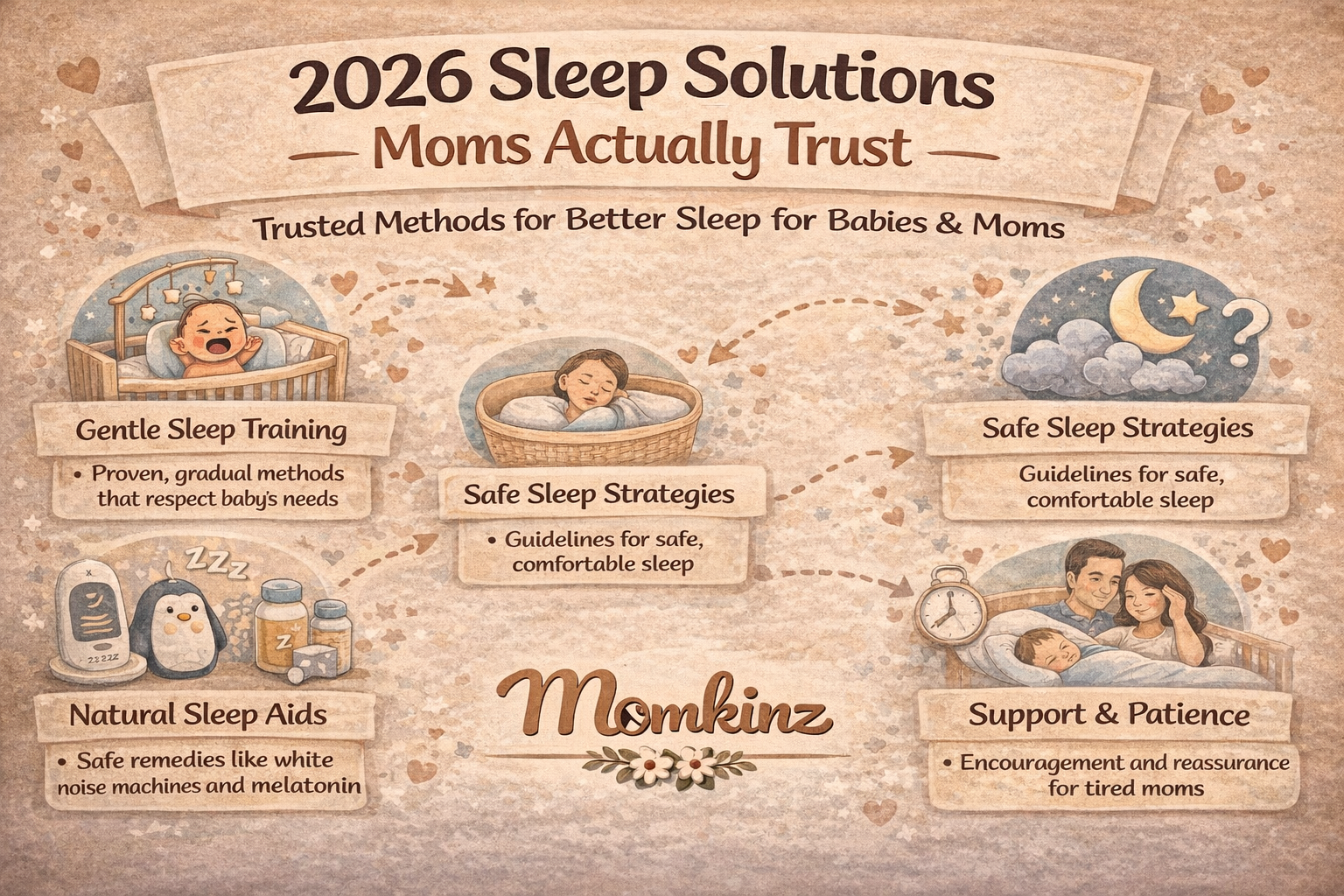
What’s Actually Helping Moms Sleep in 2026
Let’s talk about what’s truly helping, not what looks good online.
1. Letting Go of Rigid Sleep Rules
In 2026, many of us are stepping away from:
- Obsessive wake windows
- “Drowsy but awake” pressure
- One-size-fits-all schedules
Instead, we’re:
- Watching our babies’ cues
- Using flexible routines
- Allowing sleep to mature naturally
And when the pressure lifts, something shifts
Our anxiety softens, and sleep slowly improves.
2. Supporting Mom Sleep, Not Just Baby Sleep
This is a major change.
We’re finally asking:
“What do we need in order to rest?”
That looks like:
- One protected sleep block
- White noise for us, not just the baby
- A short wind-down ritual, even five minutes
- Writing fears down instead of holding them all night
One mom said:
“When I stopped forcing sleep and focused on resting my body, sleep followed.”
That wasn’t a trick.
That was nervous-system care.
What We Need to Remember About Sleep
- Sleep deprivation worsens postpartum depression symptoms
- One uninterrupted stretch can help regulate mood
- Rest still counts, even if sleep doesn’t happen
- We were never meant to do nights alone
- Recovery requires protection, not endurance
Sleep isn’t a reward.
It’s postpartum care.
“Why Can’t We Sleep Even When the Baby Sleeps?”
Because our bodies are still healing.
Because our hormones are still shifting.
Because our minds are protecting something precious.
This doesn’t mean it will always feel this way.
It means we need gentleness, not discipline.
What’s helping many of us:
- Grounding before rest (feet on the floor, slow breathing)
- Magnesium with postpartum care provider guidance
- Short mental offloads (journals, notes apps, voice memos)
- Replacing “I must sleep” with “I’m allowed to rest.”
That language change matters more than we realize.
A Real Mom Scenario (You Might See Yourself Here)
It’s 2:17 a.m.
The baby finally sleeps.
We lie down…
and our minds replay the day.
The feeds.
The worry.
At that moment, we snapped and immediately felt guilt.
We’re not failing.
We’re processing.
Sleep comes easier when emotions have somewhere to land.
What About Supplements, Tools, and Sleep Aids?
Sometimes they help when used thoughtfully.
In 2026, many of us talk with our postpartum care providers about:
- Magnesium for relaxation
- Omega-3s for mood support
- Continuing prenatal vitamins postpartum
Non-pill supports many moms prefer:
- Weighted eye masks
- Calming teas during the longest rest window
- Sleep journals to quiet the mind
- Wearable monitors to reduce constant checking
Nothing here is magic.
But support adds up.
Postpartum Telemedicine & Sleep Support: A Quiet Shift
More of us are using:
- Virtual postpartum check-ins
- Tele-lactation support for night feeding stress
- Gentle sleep coaching that centers on mental health
Postpartum support professionals are now combining:
- Sleep education
- Mood screening
- Relationship support
- Nervous-system awareness
Because sleep never exists alone.
Why Support Changes Sleep
At Momkinz, we see this again and again:
When we have:
- Postpartum support groups
- A trusted postpartum care provider
- Someone validating our exhaustion
…sleep often improves before sleep improves.
Reassurance calms the nervous system.
Calm makes rest possible.
Before We Do Anything Else, Let’s Say This
If we’re reading this while exhausted:
- We are not failing
- We are not weak
- We are not behind
- This season will change
We don’t need to solve sleep tonight.
Support Before Burnout
If sleep deprivation is affecting our mood, anxiety, or recovery, we don’t have to carry it quietly.
At Momkinz, we help moms connect with:
- Postpartum support groups near them
- Compassionate postpartum care providers
- Postpartum support professionals who understand sleep and mental health
When we’re ready, we can visit Momkinz
No pressure. Just support.
If this felt like it understood us, that matters.
We don’t need stricter rules.
We don’t need more willpower.
We need care, reassurance, and time.
Sleep will come.
Support can come now.
And we are doing better than we think.
FAQs (2026)
1. Is it normal to still feel exhausted months postpartum?
Yes. Postpartum recovery often extends far beyond six weeks.
2. Can lack of sleep increase postpartum anxiety?
Yes. Sleep deprivation is a major contributor.
3. Why can’t we nap when the baby naps?
Our nervous systems may still be on high alert.
4. Are sleep regressions permanent?
No. They are developmental and temporary.
5. Should we sleep train in 2026?
Only if it aligns with our values and mental health.
6. Does shared night care help postpartum depression?
Yes. Shared care reduces isolation and burnout.
7. Can supplements help postpartum sleep?
Sometimes, with provider guidance.
8. Is postpartum telemedicine helpful for sleep issues?
Very especially when mood symptoms are involved.
9. What’s the first step when sleep feels unbearable?
Telling someone. Support changes outcomes.
10. Where can we find postpartum sleep support?
Through Momkinz postpartum support.